Tennis Elbow – Complete Guide
By Dr. Pothireddy Surendranath Reddy
Table of Contents
- Introduction
- Epidemiology & Risk Factors
- Anatomy & Biomechanics
- Pathophysiology
- Clinical Presentation
- Diagnosis & Differential Diagnosis
- Imaging and Investigations
- Management & Treatment
- Conservative care
- Injections & advanced therapies
- Surgical options
- Rehabilitation & Exercises
- Prevention & Prognosis
- Special Considerations
- Summary
- References
1. Introduction
Tennis elbow, medically known as lateral epicondylitis or lateral epicondylalgia, is a common musculoskeletal syndrome characterized by pain over the outer (lateral) elbow. Despite its name, it often affects people who do not play tennis. Rather, repetitive overuse of the wrist extensors—especially during gripping or repetitive wrist extension tasks—leads to micro‑damage in the tendon origin on the lateral epicondyle of the humerus.
Historically, the suffix “-itis” suggests inflammation, but modern histological studies reveal that the condition is often degenerative, not inflammatory, more accurately described as a tendinosis. eMedicine+2PubMed+2
This guide provides a comprehensive, clinically relevant overview: from anatomy and mechanisms to diagnosis, management, and rehabilitation, with evidence-based references.
2. Epidemiology & Risk Factors
Prevalence
- Lateral epicondylitis affects about 1–3% of the general population, according to epidemiological studies. PubMed
- It is most common in adults aged 30–60 years. Mayo Clinic+1
Risk Factors
- Occupational: Jobs involving repeated wrist extension, gripping, or forceful use—such as carpenters, painters, plumbers, butchers, cooks. Mayo Clinic
- Recreational/sports: Racquet sports (especially tennis), poor technique, incorrect equipment. Mayo Clinic
- Intrinsic: Hypovascularity of the extensor tendon insertion may predispose to degeneration. eMedicine
- Other factors: Smoking, obesity, and certain medications have been implicated in increased risk. Mayo Clinic
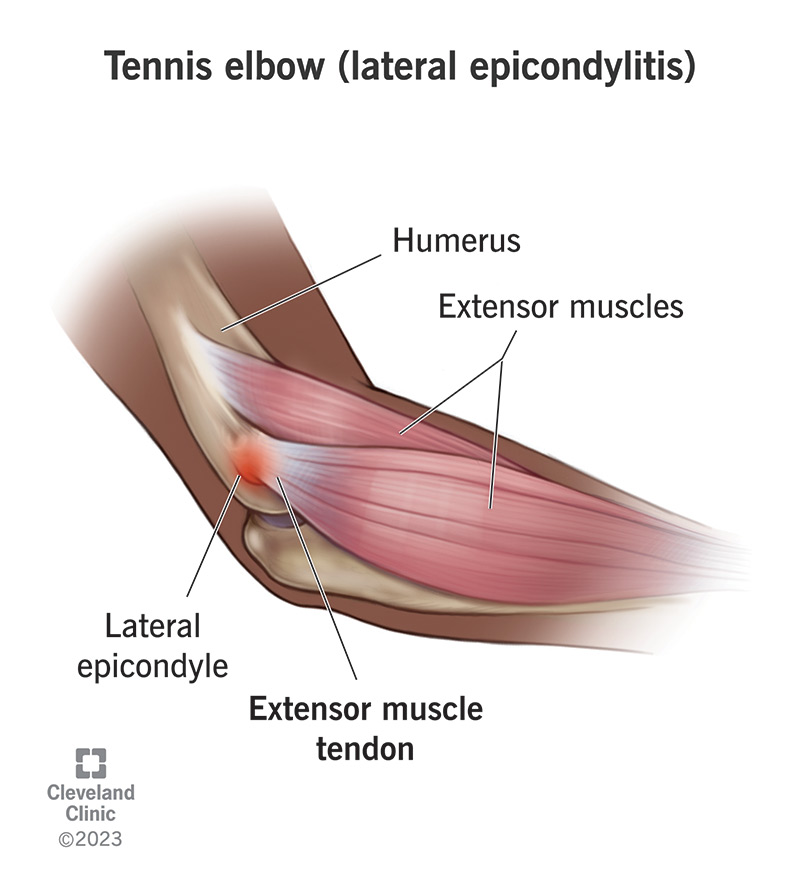
3. Anatomy & Biomechanics
Understanding the anatomy behind tennis elbow is crucial to grasp why and how it develops.
- The lateral epicondyle of the humerus is a bony prominence on the outside of the elbow. Several forearm extensor muscles originate here. PubMed+1
- The extensor carpi radialis brevis (ECRB) muscle and its tendon are most commonly implicated in tennis elbow.
- Other muscles attached to the common extensor origin include: extensor digitorum communis, extensor carpi radialis longus, extensor digiti minimi, and anconeus. PubMed
- Histological and dissection studies have shown that the ECRB tendon has a “keel-shaped” tendon structure; it interacts with surrounding structures (ligaments, joint capsule) and is subject to shearing stress during forearm movements, especially pronation, flexion, and deviation. PubMed
- The region has relatively poor vascular supply (“hypovascular zone”), which may impair tendon healing and predispose to degeneration. eMedicine
Biomechanically, during wrist extension and gripping, the ECRB tendon undergoes repeated tensile loads. When overloaded, microtears can accumulate, especially in the tendon attachment area, leading to degeneration. PubMed+1
4. Pathophysiology
- The traditional idea of inflammation (“-itis”) has shifted. Histological studies often do not show significant inflammatory cells in chronic cases. Instead, they show angiofibroblastic degeneration, collagen disarray, increased fibroblasts, and neovascularization. eMedicine
- This kind of pathology is consistent with a tendinopathy, not an acute inflammatory process. eMedicine
- Hypovascularity near the ECRB insertion likely contributes to poor healing and chronicity. eMedicine
- Repetitive mechanical overload (microtrauma) is believed to be a major driver: repeated cycles of tension during activities such as gripping or wrist extension lead to microtears, which over time accumulate and degenerate. PubMed+1
- Some studies also suggest involvement of a bursa (small fluid‑filled sac) near the radial head, which may become irritated during pronation and contribute to pain. PubMed
5. Clinical Presentation
Symptoms
- Pain on the lateral aspect (outside) of the elbow, often localized just distal to the lateral epicondyle. Mayo Clinic
- Pain may radiate into the forearm and wrist. Mayo Clinic
- Weakness in grip strength, difficulty holding objects such as cups or tools. Mayo Clinic
- Pain with common functions: shaking hands, turning doorknobs, lifting, or extending wrist. Mayo Clinic
- In chronic cases, stiffness or limited function may develop.
Onset and Course
- Usually insidious onset, associated with repetitive tasks. Mayo Clinic
- Symptoms may worsen gradually; some patients may recall a precipitating activity, but many do not. Mayo Clinic
- The natural course is variable: many cases improve with conservative care, but some persist for months or more.
6. Diagnosis & Differential Diagnosis
Diagnosis
- Primarily clinical, based on history and physical exam. Mayo Clinic+1
- On examination: point tenderness over the lateral epicondyle, pain with resisted wrist extension, pain on gripping. PubMed
- Special tests: Cozen’s test (resisted wrist extension), Mill’s test (passive wrist flexion with elbow extended), and others.
Differential Diagnosis
Clinicians should consider other causes of lateral elbow pain:
- Radial tunnel syndrome / posterior interosseous nerve entrapment
- Osteoarthritis of the elbow
- Lateral collateral ligament injury
- Joint or tendon tear
- Cervical radiculopathy (referred pain)
- Biceps or triceps tendon pathology (less common)
If symptoms persist despite treatment, or if there are red flags, further work-up may be needed.
7. Imaging and Investigations
- Plain radiographs (X-ray): may be indicated to rule out joint changes, osteoarthritis, bony abnormalities, or calcification. NCBI
- Ultrasound: can help visualize tendon thickening, tears, or neovascularization.
- MRI: used in refractory cases to evaluate for partial tendon tears, intra-substance degeneration. Mayo Clinic
- Electrodiagnostic studies (EMG/NCV): occasionally considered if nerve entrapment is suspected. Mayo Clinic
- Biopsy or histology is not routinely performed but from prior studies, microscopic pathology shows tendinosis rather than inflammation. eMedicine
8. Management & Treatment
Management of tennis elbow involves a spectrum: from conservative therapy to more invasive options, depending on severity, duration, and response.
8.1 Conservative Care
Rest & Activity Modification
- Avoid or modify activities that exacerbate pain; reduce repetitive wrist extension and gripping. Mayo Clinic
- Educate patients on ergonomics and technique (sports or occupational) to reduce tendon load.
Physical Therapy
- Exercises to strengthen and stretch the forearm extensors: typically eccentric loading exercises are very effective. IJCRT+1
- Manual therapy, mobilization, and sometimes other modalities (ultrasound, low-level laser) may help. PubMed
- Use of counter-force bracing (a strap worn around the forearm) to reduce tendon stress during activity. NCBI+1
Pharmacologic Pain Relief
- NSAIDs: oral or topical for pain management. NCBI
- Cold therapy (ice): applied for 10–15 minutes after activity. Mayo Clinic
Other Conservative Modalities
- Thermal (heat) and electrical agents (e.g., TENS) have been used. PMC
- Acupuncture: some moderate evidence supports benefit without the side effects of steroids. PubMed
- Low-level laser therapy: emerging as a potential aid. PubMed
Evidence Considerations
- A critical review of conservative therapies noted that while steroid injections are common, they carry risk of recurrence and tissue changes; alternative therapies like acupuncture and ultrasound have lower risk but need more robust evidence. PubMed
- A more recent review highlighted that physiotherapy, load management, and modalities can be effective. PMC
8.2 Injections & Advanced Therapies
When conservative treatment fails or pain persists, more advanced therapies may be considered:
Corticosteroid Injections
- Often used for short-term pain relief. Mayo Clinic
- However, repeated steroid injections are controversial because of potential tendon weakening and high recurrence. PubMed
Platelet‑Rich Plasma (PRP) Injections
- PRP has gained popularity: uses patient’s own platelets to promote tendon healing. Mayo Clinic
- Mixed evidence, but many clinicians prefer it over steroids due to potential for more durable healing.
Dry Needling / Fenestration
- Dry needling: repeated puncture of the degenerated tendon to stimulate healing. Mayo Clinic
- Needle fenestration (often under ultrasound): uses a needle to make multiple small perforations in the tendon to provoke a healing response. Mayo Clinic
Ultrasonic Tenotomy (e.g., TENEX)
- Minimally invasive: under ultrasound, a special vibrating needle breaks down degenerative tissue which is then aspirated. Mayo Clinic
Extracorporeal Shock Wave Therapy (ESWT)
- Shock waves delivered to the tendon to stimulate healing. Mayo Clinic
- Evidence is varied; some patients respond well, others less so.
Prolotherapy / Irritant Injection
- Injection of solutions like hypertonic dextrose or saline to trigger a healing response. Mayo Clinic
Surgical Options
When non-surgical care fails (typically after 6–12 months), surgery may be considered:
- Open surgery: excision of diseased tendon tissue and decortication (creating small holes in bone to enhance blood flow) at the lateral epicondyle. PubMed
- Arthroscopic surgery: minimally invasive; removal or debridement of degenerative tendon tissue under arthroscopy. Mayo Clinic
- Denervation: less common; releasing sensory nerves to reduce pain. SpringerLink
Outcomes from surgical series are generally good, especially when conservative treatment has failed. PubMed+1
9. Rehabilitation & Exercises
Rehabilitation is a cornerstone of recovery. A structured, progressive exercise program helps not just in pain relief but in tendon remodeling.
Exercise Principles
- Eccentric strengthening: slow, controlled lengthening of the tendon under load. Very effective in tendinopathy. IJCRT+1
- Isometric exercises: holding the tendon under tension without changing length can reduce pain in early stages.
- Concentric strengthening: once pain allows, build up traditional strengthening along with eccentric work.
- Stretching: wrist extensor stretches to maintain soft tissue flexibility.
- Scapular and kinetic chain training: strengthening shoulder, core, and proximal muscles since the elbow does not work in isolation. Many modern rehab protocols emphasize the kinetic chain. Reddit
Protocol Example
- Phase 1 (Acute / Pain Reduction):
- Isometric holds (e.g., wrist extension) 3 × 45 seconds, 2–3 times/day
- Gentle stretching after isometrics
- Ice after exercise
- Phase 2 (Reactive / Early Remodeling):
- Eccentric wrist extension: 3 sets × 15 reps, once or twice daily, with light weight
- Continue stretching and isometrics
- Use counter‑force brace during aggravating activities
- Phase 3 (Remodeling & Strengthening):
- Increase load gradually on eccentric exercise
- Add concentric reps and more functional exercises (grip, lifting)
- Shoulder and scapular strengthening
- Phase 4 (Return to Activity / Prevention):
- Sport- or job-specific strengthening
- Load management strategies
- Ongoing maintenance exercises
Modalities During Rehab
- Ultrasound, low‑level laser, and shockwave therapy might be used adjunctively. PubMed+1
- Education on load management, rest, and technique is crucial.
10. Prevention & Prognosis
Prevention
- Ergonomic assessment: for both sport (tennis) and work-related tasks.
- Use of proper technique, especially in sports: coaching, racquet grip size, string tension, and stroke mechanics.
- Strengthening and conditioning: maintain forearm, shoulder, and core strength to distribute load.
- Use of braces: counter‑force straps during repetitive tasks to offload tendon. NCBI
- Optimize rest and recovery: avoid overuse, incorporate rest cycles.
Prognosis
- Many cases improve with conservative care, though recovery may take several months. Mayo Clinic
- Recurrence is common if underlying load issues are not addressed.
- Surgical outcomes are generally favorable in those who do not respond to non-operative treatment. PubMed
- With proper rehabilitation, recurrence can be minimized and function restored.
11. Special Considerations
- Occupational Cases: In work-related epicondylitis, coordination with occupational therapy and workplace ergonomics is essential.
- Athletes: Return-to-sport decision-making must include assessment of technique, equipment, and load tolerance.
- Comorbidities: Conditions like arthritis or nerve entrapment may complicate management.
- Chronic/Recalcitrant Cases: For persistent symptoms, imaging (MRI/ultrasound) and advanced treatment (PRP, shockwave, surgery) may be indicated.
- Older Adults: Healing may be slower; tendon degeneration may be more advanced.
- Patient Education: Explaining the “tendinopathy” model (degeneration rather than inflammation) helps set realistic expectations and promotes adherence to rehab.
12. Summary
- Tennis elbow (lateral epicondylitis) is a common overuse injury affecting the extensor tendons at the lateral epicondyle.
- Despite its name, it frequently occurs in non-athletes, especially those doing repetitive wrist extension or gripping tasks.
- Histopathology shows degenerative changes (tendinosis), not just inflammation.
- Diagnosis is clinical, though imaging may be useful in persistent or atypical cases.
- Conservative management (rest, physical therapy, counter‑force bracing) is first-line.
- Injections (PRP, steroids), dry needling, and shockwave therapy are options for refractory cases.
- Surgical intervention is reserved for chronic, non-responsive cases and has good outcomes.
- Rehabilitation must be structured and progressive, with emphasis on load management, eccentric exercise, and kinetic chain strengthening.
- Prevention strategies and patient education are vital to reduce recurrence and promote long-term recovery.
13. References
- Mayo Clinic. Tennis elbow – Symptoms and causes. Mayo Clinic. Mayo Clinic
- Mayo Clinic. Tennis elbow – Diagnosis & treatment. Mayo Clinic
- PubMed. A critical review of the current conservative therapies for tennis elbow (lateral epicondylitis). PubMed
- PubMed. Tennis elbow: a review. PubMed
- PubMed. Lateral epicondylitis. A review of structures associated with tennis elbow. PubMed
- PubMed. Lateral epicondylitis (tennis elbow): nonsurgical vs surgical outcomes. PubMed
- PubMed. LATERAL EPICONDYLITIS OF THE ELBOW. PubMed
- PubMed (PMC). Conservative Management of Lateral Epicondylalgia: A Review. PMC+1
- Medscape. Lateral Epicondylitis: Practice Essentials, Anatomy, Pathophysiology. eMedicine
- StatPearls. Lateral Epicondylitis. NCBI
- Springer. Tennis Elbow: Clinical Management (eBook). SpringerLink
- IJCRT Case Report. Eccentric strengthening exercise case in lateral epicondylosis. IJCRT
1. https://pothireddysurendranathreddy.blogspot.com/2025/11/hip-pain-complete-guide-to.html
Hip Pain
2. https://pothireddysurendranathreddy.blogspot.com/2025/11/oldage-osteoporosis-management-by.html osteoporosis
3. https://pothireddysurendranathreddy.blogspot.com/2025/11/knee-pain-management-by-drpothireddy.html knee pain
- Get link
- X
- Other Apps
- Get link
- X
- Other Apps

Comments
Post a Comment